Vitamin D: Bioenergetic Wunderkind or Arbiter of Doom?
"What could be more important to understand than biological energy? Thought, growth, movement, every philosophical and practical issue involves the nature of biological energy." — Raymond Peat
Table of Contents
Argument #1: “25-D is The Biologically Inactive Storage Form of Vitamin D”
Argument #4: “You Need The Active Form of Vitamin D to Activate The Vitamin D Receptor (VDR)”
Argument #5: “You Need The Active Form of Vitamin D to Activate The Immune System”
Argument #6: “Taking a Vitamin D Supplement Gave Me Symptoms”
Argument #7: “You’re Only Supposed to Get Vitamin D From The Sun”
Argument #8: “25-D Deficiency is Actually A Magnesium Deficiency”
Argument #9: “Vitamin D Supplementation Depletes Vitamin A, Vitamin K, and Copper”
Argument #10: “Vitamin D Has Gone Mainstream and is Part of an Agenda to Poison You”
Argument #11: “Just Because a Substance Lowers a Stress Hormone Doesn’t Make it Good”
Glossary
Definitions paraphrased from raypeat.com
Thyroid: Thyroid hormone is necessary for respiration on the cellular level, and makes possible all higher biological functions. Without the metabolic efficiency, which is promoted by thyroid hormone, life couldn’t get much beyond the single-cell stage. Without adequate thyroid, we become sluggish, clumsy, cold, anemic, and subject to infections, heart disease, headaches, cancer, and many other diseases, and seem to be prematurely aged, because none of our tissues can function normally.
Progesterone: Progesterone, because of its normal anesthetic function, directly quiets nerves, and in this way suppresses many of the excitotoxic processes. It has direct effects on mitochondria, promoting energy production, and it facilitates thyroid hormone functions in various ways. It promotes the elimination of estrogen from tissues, and is a "diuretic" in several benign ways, that are compatible with maintenance of blood volume. The effects of estrogen and progesterone are systemically opposed to each other—estrogen excites, progesterone calms, estrogen cools, progesterone heats, estrogen increases nitric oxide, progesterone lowers it, etc
Parathyroid Hormone (PTH): The parathyroid hormone (PTH) is an important regulator of calcium metabolism. If dietary calcium isn't sufficient, causing blood calcium to decrease, the PTH increases, and removes calcium from bones to maintain a normal amount in the blood. PTH has many other effects, contributing to inflammation, calcification of soft tissues, and decreased respiratory energy production.
Prolactin: Prolactin is a hormone secreted by the pituitary gland during pregnancy, and during stress. It promotes milk production, removes calcium from the bones, and inhibits progesterone formation. Prolactin acts on the thyroid gland to decrease its activity, and on other tissues to increase their glycolysis (with lactate production), while decreasing oxidative metabolism.
Serotonin: Serotonin is a mediator of inflammation that suppresses metabolism, disturbs blood pressure, and promotes clotting, so it would be a Manichean-seeming misfortune if it was also essential to have lots of it to experience euphoria. But in reality a state of 'serotonergia' is a state of torpor, discomfort, and depression, rather than a state of alert pleasure
Aldosterone: One of the things that happen when there isn't enough sodium in the diet is that more aldosterone is synthesized. Aldosterone causes less sodium to be lost in the urine and sweat, but it achieves that at the expense of the increased loss of potassium, magnesium, and probably calcium. Aldosterone secretion increases during the night, and its rise is greater in depressed and stressed people. It inhibits energy metabolism, increases insulin resistance, and increases the formation of proinflammatory substances in fat cells. During aging, salt restriction can produce an exaggerated nocturnal rise in aldosterone.
Introduction
This post will be an aggregation of the content that’s been released on several social media channels. In short, I’m keen on defending vitamin D (cholecalciferol) because, in my own experience, it’s been incredibly useful (maybe one of the most useful supplements I’ve ever used) and fits in nicely with thyroid hormone, progesterone, CO2, sugar, salt, gelatin, aspirin, etc., as a basic anti-stress, anti-inflammatory, and pro-energy therapy.
Something I want to make really clear is that I’m 100% in solidarity with people that believe that a vitamin D supplement harmed them in some way.
My view is that all supplements, especially ones containing silica, MCT oil, gums, citric acid, titanium dioxide, carrageenan, etc., are potential intestinal irritants that can cause symptoms. For myself, I use liquid vitamin D made from lanolin only on my skin. So, again, I’m not defending all the shitty vitamin D supplements out there.
(My negative experience with many supplements caused me to ask Ray Peat to join me for a podcast about the subject in 2016.)
Another thing is that this article is not to convince you, the reader, to take vitamin D. This article is primarily about defending vitamin D against the laughable incoherent hyperbole that has developed over the last year or so (‘vitamin D is as bad as fish oil and will calcify you’).
The third important thing is that I’m addressing these points of contention from a bioenergetic point of view — or the idea that good health is sustained by the intensity at which protein, carbohydrate, and fat are reduced down into electrons that are continuously flowing through the living cell to be ultimately vacuumed up by oxygen (with the help of carbon dioxide) resulting in ATP, water, and carbon dioxide.
"The organizing power of energy flow is hypothesized to be the origin of biological complexity and its decline the basis of "complex" diseases and aging...”
“This bioenergetic perspective on disease provides a unifying pathophysiological and genetic mechanism for neuropsychiatric diseases such as Alzheimer and Parkinson Disease, metabolic diseases such as diabetes and obesity, autoimmune diseases, aging, and cancer...”
—Wallace, D.C. Bioenergetic origins of complexity and disease. (2011)
I believe that the bioenergetic worldview that Albert Szent-Györgyi, Hans Selye, Otto Warburg, Gilbert Ling, Ray Peat, and others have helped establish is coherent, and catastrophic errors are less likely when evaluating a substance’s promotion or inhibition of mitochondrial respiration.
I’m unaware of the context for health and disease of various anti-vitamin D people are on the internet, but this is paramount for understanding the points made in this article.
The Anti-Vitamin D Argument Steelman
As I understand the basic argument, it goes a little something like this:
Vitamin D3 or cholecalciferol is converted into the non-biologically active storage form of vitamin D (calcifediol or 25-D) by the liver, which is converted again into the biologically active calcitriol (1,25-D) primarily by the kidneys.
Since 1,25-D is barely ever measured, you could be sufficient in it already; thus, randomly supplementing with cholecalciferol to increase 25-D is risky and could cause harm.
1,25-D is the only form of vitamin D that activates the vitamin D receptor (VDR), which is responsible for all of vitamin D’s useful biological functions. For instance, 1,25-D is essential for mounting an immune response.’
From here on out, we’ll be deconstructing these arguments from a bioenergetic point of view.
Argument #1: “25-D is The Biologically Inactive Storage Form of Vitamin D”
This is the heart of the argument as it’s claimed that ‘all the accolades’ of vitamin D belong to active 1,25-D, not 25-D, which is said to be ‘biologically inactive.’
This one, in my estimation, is quite bizarre as 25-D has so many anti-stress, anti-inflammatory, and pro-mitochondrial energy effects.
For example, increasing 25-D with supplemental cholecalciferol has been shown to oppose the negative effects of parathyroid hormone (PTH), serotonin, prolactin, aldosterone, and cortisol — which all interfere with energy production:
25-D Lowers PTH
PTH Context: “PTH inhibited mitochondrial respiration… The reduction of oxidative phosphorylation may result in decreased ATP synthesis. These events may cause long-term adverse effects of PTH on the myocardium…” — Rodriguez, et al. (2009)
"Optimal vitamin D status, defined by estimated maximum PTH suppression, does not occur until at least 25-D levels ≥40 ng/ml [100 nmol/l].” — Ginde, et al. (2012)
“In healthy persons, the reference (normal) range for serum PTH is known to decline as serum 25-D levels increase. Therefore, the theoretical plateau in PTH, as 25-D increases, can be used as a determinant in establishing the adequacy of vitamin D status.” — Muscogiuri G., et al. (2014)
PTH Increases Serotonin, Prolactin, and Aldosterone
Serotonin Context: “...We argue that the evolved function of the serotonergic system is energy regulation—which we define as the coordination of metabolic processes with the storage, mobilization, distribution, production and utilization of energetic resources to meet adaptive demands.” Andrews, et al. (2015)
“Release of serotonin and histamine was demonstrated with 25 units/ml PTH or higher.” … “These results demonstrate that elevated levels of PTH can induce mast cell secretion in vitro and in vivo and suggest a possible role for mast cells in the pathophysiology of non-allergic disease states.” — Tsakolos, et al. (1983)
“…Our results suggest that serotonin could be one of the factors regulating PTH secretion and/or contributing to PTH hypersecretion in various forms of primary hyperparathyroidism.” — Zimmerman, et al. (1980)
Prolactin Context: “A conclusion has been made that one of the most important mechanisms of the adaptive effect of prolactin is its ability to suppress thyroid function, thus decreasing the metabolism level, which results in reduction of oxygen consumption…” — Strishkov, V.V. (1991)
“These results show that an excess of plasma prolactin is associated with an excess of plasma PTH and vice versa.” — Raymond, et al. (1982)
Aldosterone Context: “Adrenocortical hormones which stimulate inflammation, as for example, aldosterone… They have a marked effect on mineral metabolism, and are therefore known as mineralcoritcoids.” … “There is ample evidence of increased ACTH, cortisol, and, under certain circumstances, even aldosterone secretion as a consequence of fear and anxiety, for example, in students during oral examinations and in preoperative patients.” — The Stress of Life by Hans Selye (1984)
“Growing evidence points to a bi-directional and positive relationship between the renin-angiotensin-aldosterone system and PTH.” …“Hyperaldosteronism and hyperparathyroidism represent pathophysiologic conditions that may contribute to or perpetuate each other; aldosterone regulates parathyroid hormone and associates with adverse skeletal complications, and parathyroid hormone regulates aldosterone and associates with adverse cardiovascular complications.” — Vaidya, et al. (2015)
25-D Opposes Prolactin
“Cholecalciferol administered to patients with macroprolactinemia increased 25-D, reduced total prolactin and macroprolactin, as well tended to reduce PTH…” — Krysiak, et al. (2015)
“Female patients with prolactinoma have lower 25-D levels and have higher prevalence of 25-D insufficiency and deficiency among prolactinoma patients when compared with normal subjects. Also 25-D deficiency in prolactinoma patients associated with larger adenoma size and higher prolactin level.” — Aboelnaga, et al. (2017)
25-D Lowers Aldosterone
“The findings indicate that cholecalciferol supplementation significantly decreases [plasma aldosterone concentration] in patients with arterial hypertension and 25-D insufficiency.” — Grübler, et al. (2016)
“Cholecalciferol repletion decreases aldosterone in patients with heart failure and low serum 25-D.” — Boxer, et al. (2014)
“The co-existence of 25-D deficiency and elevated levels of aldosterone in benign prostate hyperplasia, presented for the first time in literature, strongly favors a link between the renin-angiotensin-aldosterone system, vitamin D and benign prostate hyperplasia pathogenesis.” — Yalçınkaya, et al. (2014)
25-D Opposes Cortisol
“…In the present investigation we further confirmed the importance of sufficient 25-D availability in maintaining proper function of hepatic cells in normal and diseased conditions. It has been demonstrated that prednisolone-induced oxidative/nitrosative stress and liver injury may be related to established inadequate circulating level of 25-D, because prohormone repletion after cholecalciferol treatment resulted in partial or complete normalization of the most detrimental alterations associated with glucocorticoid hepatotoxicity.” — Lisakovska, et al. (2016)
Moreover, 25-D synergizes with progesterone and thyroid hormone:
25-D Synergizes with Progesterone
“In this context something as simple as providing cholecalciferol supplementation could improve recovery and potentially enhance the neuroprotective benefits of progesterone (or any other) treatment.” … “…Progesterone and 25-D each work through different pathways to reduce cellular injury and enhance the metabolic processes of repair…” — Cekic M., et al. (2009)
25-D Synergizes with Thyroid
“Our results indicated that patients with hypothyroidism suffered from hypovitaminosis D with hypocalcaemia. Moreover, the positive significant correlation between each of 25-D and calcium with thyroid hormones and that negative significant correlation with TSH levels, suggested that deficiency of serum 25-D and calcium levels were significantly associated with degree and severity of the hypothyroidism which encourage the advisability of cholecalciferol supplementation. Screening for 25-D deficiency and serum calcium levels recommended for all hypothyroid patients.” — Mackawy A., et al. (2013)




While 25-D helps to oppose and terminate the stress response, 1,25-D appears to amplify it:
1,25-D Increases Prolactin:
“The results confirm the stimulating action of 1,25-D on prolactin secretion in healthy women...” — Zofkova, et al. (1988)
“Administration of prolactin to animals produces an increase in the 1a-hydroxylase activity and a rise in plasma 1,25-D. Consistent with a possible regulatory role of prolactin on 1,25-D biogenesis, the administration of bromocriptine, which suppresses prolactin secretion, lowers plasma 1,25-D values in lactating rats. These findings suggest prolactin-mediated modulation of 1a-hydroxylase activity...” — Rosen, et al. (1983)
“Because a high-calcium diet results in the suppression of 1,25-Dproduction, these results indicate that prolactin may require the presence of 1,25-D to exert its long-term stimulatory effect on intestinal calcium absorption…” — Charoenphandhu, et al. (2006)
“…It now seems that the renal hydroxylation is under the control of prolactin and this may account for the dramatic changes in calcium metabolism in pregnancy and lactation.” — Horrobin (1979)
1,25-D Synergizes with Estrogen
“Elevated 1,25-D levels are observed during pregnancy and estrogen therapy.” “…Both the total and free 1,25-D levels are elevated during pregnancy and estrogen therapy.” — Osteoporosis 4th Edition by Marcus, et al. (2013)
“Estrogen increases intestinal calcium absorption in postmenopausal women by preserving the normal intestinal responsiveness to 1,25-D.” — Calcium Throughout the Life Cycle by Bess Dawson-Hughes (2006)
The idea that 1,25-D is essential for activating the vitamin D receptor and stimulating the immune system will be covered in parts #4 and #5.
Argument #2: “Increasing 25-D Increases Active 1,25-D”
Another significant grievance of the anti-vitamin D crowd is that since 1,25-D is never measured — you might already be sufficient in it. Thus, supplementing with cholecalciferol to increase 25-D, which converts into 1,25-D, is risky.
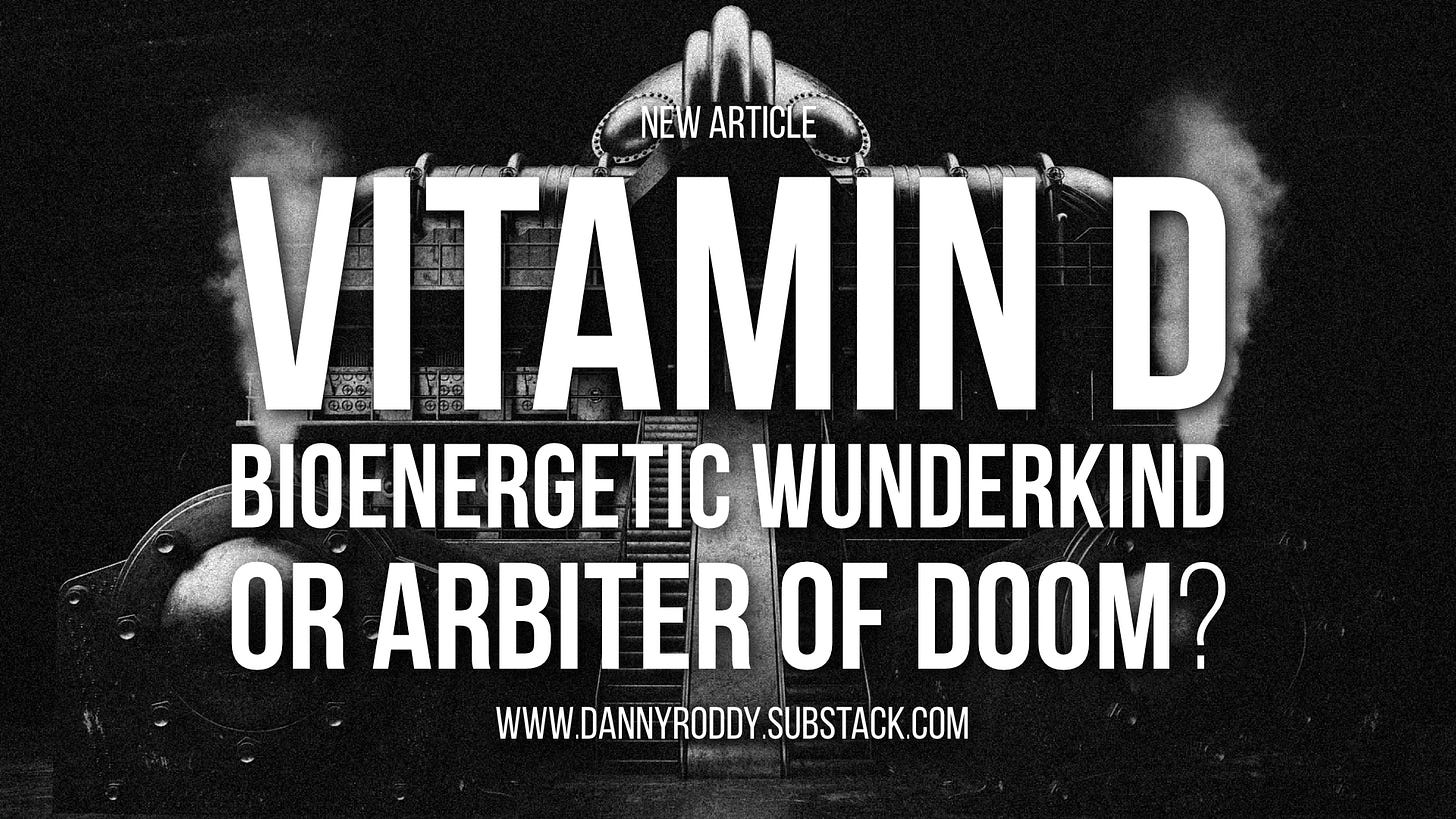
While viewing chemistry charts might make a person think that 1,25-D is the ultimate destination for 25-D, however, in the living organism, at physiological amounts, the 1a-hydroxylase enzyme that converts 25-D to 1,25-D tends to decrease when supplementing 25-D.
The 1a-hydroxylase enzyme is turned on in various emergency situations, primarily by parathyroid hormone (PTH), which tends to increase in a calcium deficiency, 25-D deficiency, phosphorus excess, or cortisol excess:
1,25-D Regulators: PTH, Calcium, Phosphate, Etc.
“There seems to be universal agreement that PTH is the major regulator [of kidney 1a-hydroxylase]. Plasma 1,25-D is elevated by hyperparathyroidism even when there is concurrent hypercalcemia. The 1,25-D falls after parathyroidectomy despite the hypocalcemia.”
“The kidneys contain a 25-D 1a-hydroxylase that catalyzes the conversion of 25-D to 1,25-D. The reaction is controlled by parathyroid hormone (PTH), by phosphate, and calcium levels, and by several other regulators.”
“Glucocorticoids acutely elevate plasma calcium, probably because they stimulate parathyroid hormone secretion and thereby accelerate production of 1,25-D.” — Endocrine Physiology by Constance R. Martin (1985)
“…We speculate that the decrease in plasma 25-D diminishes the suppressive effect on PTH expression in the parathyroid gland, with the resultant increase in plasma PTH and secondary hyperparathyroidism. The normal or even elevated level of bioactive 1,25-D may be due to a compensatory mechanism such that the increased PTH enhances the expression of 1a-hydroxylase in the kidney and facilitates systemic conversion from 25-D to 1,25-D to maintain intestinal calcium absorption.” — Kawahara, et al. (2008)
1,25-D Causes Hypercalcemia and Calcification
"Severe hypercalcemia is mainly caused by inappropriately high concentrations of compounds which promote bone resorption, in particular PTH, PTHrP, or 1,25-D." — Schmind, C. (1994)
“Replacement therapy with calcitriol… often produces hypercalcaemia… In addition, these vitamin D compounds can aggravate the hyperphosphataemia in these patients.” — Brown, et al. (2002)
25-D Lowers 1,25-D
“...With high dose cholecalciferol therapy... PTH is physiologically down-regulated and therefore the synthesis of 1,25-D and dietary calcium absorption are reduced.” — Vaidya, et al. (2015)
Gigantic Cholecalciferol Dose Causes Transient Increase in 1,25-D
“Twenty-five patients with vitamin D deficiency… randomly received either 540,000 IU of cholecalciferol… or matched placebo…” … “As serum PTH and total calcium levels, which both modulate CYP27B1 activity, remained unchanged during that period, it seems that this transient rise in 1,25-D was mainly attributable to the boost of suddenly available 25-D substrate. A plausible reason for the subsequent decrease in 1,25-D levels following day 3 may be the induction of CYP24 hydroxylase gene that shifts 25-D more towards the production of inactive 24,25 (OH)2D thus limiting the rise of 1,25-D levels.” — Amrein, et al. (2011)
Calcium Lowers 1,25-D
“Oral calcium supplementation in these men was also accompanied by a reduction in the plasma concentration of PTH and 1,25-D...” — Lijnen, et al. (1995)
“...Oral calcium supplementation is accompanied by a reduction in the intracellular free and total calcium… and by a decrease in the plasma concentration of PTH and 1,25-D.” —Petrox, et al. (1999)
“Only minute quantities of 1,25-D are made in well-fed individuals... They can rise several fold when the diet is calcium-deficient...
It is possible to adapt to diets that differ widely in calcium content by making compensatory adjustments of the 1a-hydroxylase activity. Usually, the circulating 1,25-D levels vary inversely with the calcium supply.”
“The role of 1,25-D in calcium conservation has been likened to the role of aldosterone in sodium conservation...” — Endocrine Physiology by Constance R. Martin (1985)
“Hypocalcemia caused by calcium-deficient diets, 25-D deficiency, or pathological factors results in increased production of 1,25-D. This hypocalcemic-mediated induction of 1,25-D production is secondary to increased PTH. Administration of PTH to animals results in increased 1,25-D production.” — Pike, et al. (2005)
PTH Increases Loss of 25-D
“In the disease state of hyperparathyroidism, the greatly elevated concentration of PTH in blood results in increased loss of 25-D mediated by the increased renal production of 1,25-D, which activates the hepatic uptake and destruction of 25-D.” — Rybchyn, et al. (2020)
Elevated PTH is Common
“The incidence of primary hyperparathyroidism in Denmark continues its remarkable rise.” —Abood, et al. (2013)
“…In older persons the presence of serum PTH levels within the upper normal range is highly related to cardiovascular disease.” — Buizert, et al. (2013)
“…It is important to point out that low levels of parathyroid hormone (PTH) are essential for maintaining healthy bone structure and normal remodeling.” — Endocrine Physiology Constance R. Martin (1985)
PTH is Associated with Metabolic Syndrome, Depression, Anxiety, and Trauma
“The PTH level... is an independent predictor of metabolic syndrome...” — Hjelmesaeth, et al. (2009)
“In addition, increased PTH levels were highly correlated with levels of emotional and physical abuse and neglect.” …“Levels of PTH correlated with several clinical characteristics, including the diagnosis of bipolar disorder… psychotic symptoms… suicidality, total number of acute episodes and of hospitalizations… aggressive behaviors… higher childhood trauma…” — Steardo, et al. (2021)
“Vitamin D deficiency, anxiety and depression symptoms are commonly associated with chronic functional constipation induced by intestinal motility disorders.” … “Patients with delayed transit time of both intestinal tracts… showed significantly reduced levels of vitamin D and higher PTH levels and showed worsening quality of life.” — Panarese, et al. (2019)
How is that possible? Doesn’t taking a precursor result in more of the metabolite?
I don’t think so.
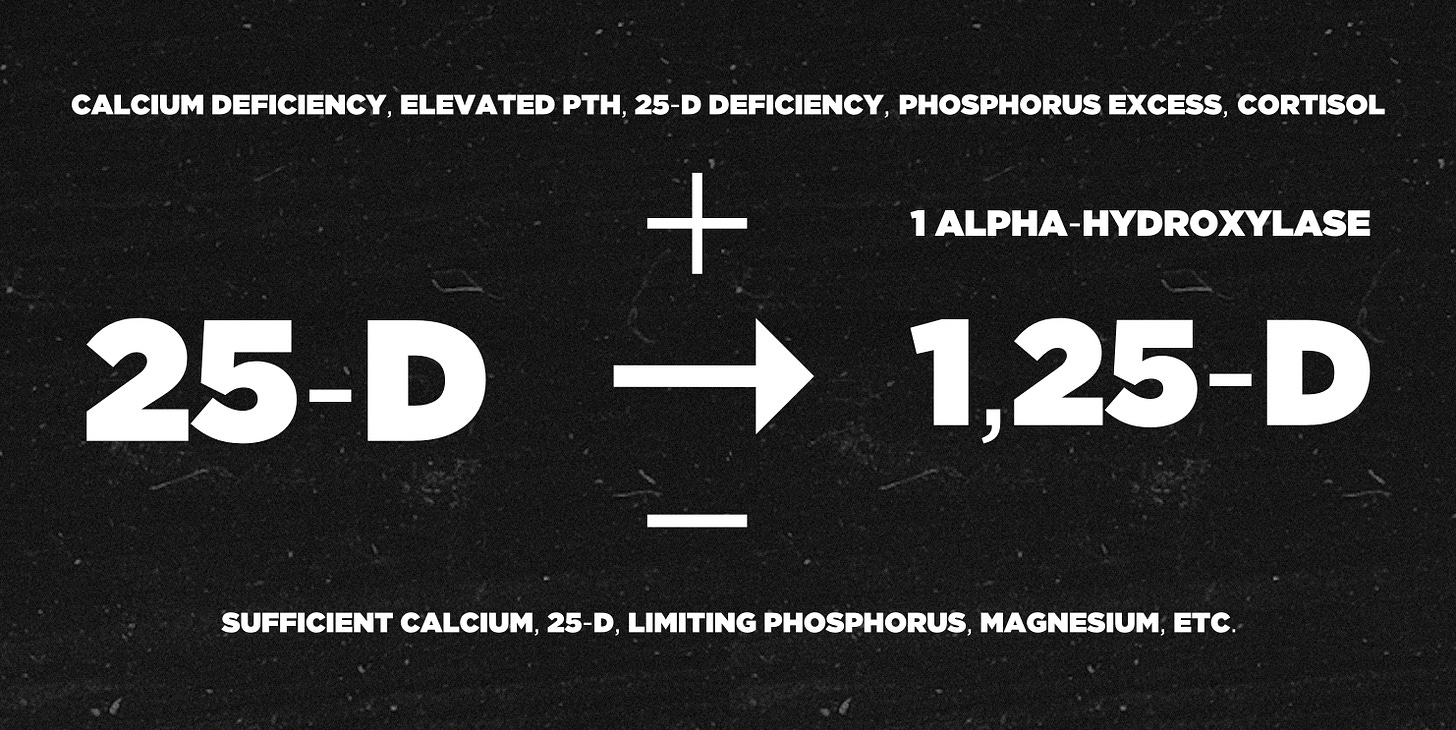
For example, the relationship between the “youth-associated” steroids pregnenolone and progesterone and their downstream metabolites cortisol and aldosterone.
By looking at a hormone chart, a person would be led to believe that taking pregnenolone or progesterone would increase cortisol and aldosterone. However, the opposite is true.
Taking Pregnenolone and Progesterone Decreases Downstream Metabolites
“...Corticotropin-releasing hormone (CRH)… is a key regulator of hypothalamic-pituitary-adrenal (HPA) axis activity during stress. CRH via pituitary adrenocorticotropic hormone (ACTH) stimulates glucocorticoid synthesis and release from adrenal glands.” “...In the present study, we found that some neurosteroids in a concentration-dependent manner inhibited CRH… Among investigated neurosteroids, pregnenolone, the main precursor of steroid hormones, exerted the most potent effect.” —Budziszewska, et al. (2010)
“Animal studies suggest that neuroactive steroids, in particular progesterone and its metabolites, have stress-dampening effects… Progesterone 50 mg attenuated peak increases in plasma cortisol and reduced changes in negative mood and alertness after stress…” —Childs, et al. (2010)
“These results were interpreted as demonstrating that progesterone is an antagonist of aldosterone…” — Landau, et al. (1958)
“The concept of negative feedback regulation by prohormone via intracellular activation is analogous to that of the negative feedback regulation of TSH by thyroid hormone. It has been known that 5′-deiodinase type II, which converts T4 to T3, is highly expressed in thyrotroph in the pituitary, and the enzyme controls and mediates T4-induced TSH suppression. Thus, we assume that 1a-hydroxylase, which converts 25-D to 1,25-D, plays a similar role in the negative feedback regulation of PTH gene by 25-D in the parathyroid gland.” — Kawahara, et al. (2008)
As Ray Peat mentioned in his interview with Kate Deering, the lack of a basic stabilizing factor such as thyroid, pregnenolone, progesterone, or 25-D can cause an emergency compensatory effect, which tends to be mediated by an older, more primitive substance that increases entropy.
“Nature develops its structures stepwise, adding to them and improving them gradually, never throwing away the foundation.” …“The ability of unlimited proliferation is an attribute of life. In the simplest living forms growth is limited only by environmental factors. In multicellular organisms this potential has to be suppressed in the interest of the organism as a whole.” — The Living State by Albert Szent-Györgyi (1972)
Argument #3: “Vitamin D is Rat Poison”
This is probably the most common ‘shock and awe’ argument indiscriminately thrown around in comment sections of the alt health world. And it seems compelling — as all a person has to do is look up rodenticides to find that cholecalciferol is, in fact, the primary ingredient in some rat poisons.
To put things into perspective, let’s take the popular rodenticide d-Con. According to d-Con’s marketing material, each gram of their soft bait contains about 31,428 IUs of cholecalciferol. It takes 0.5 milligrams of bait per kilogram of body weight to increase serum calcium and phosphorus enough to cause tissue mineralization and kidney failure.
So, if a rat were 250 grams (0.5 lbs), it would take about 3,928 IUs of cholecalciferol to induce death, which doesn’t sound like much.
However, in a 75-kilogram human (~165 lbs), d-Con’s recommended dose would be 1,178,550 IUs.
Some people might think taking a million units of cholecalciferol would lead to instant death, but in 2016, a toxicity report was released that documented one person accidentally ingesting over 1,800,000 IUs a day for over two months and another who used 900,000 IUs for one month:
“…Both developed symptomatic hypercalcemia, with markedly elevated 25-D blood levels peaking at 1220 and 645 ng/ml, and both recovered uneventfully after stopping the vitamin D. The hypercalcemia was noted to resolve in both once the 25-D blood levels fell below 400 ng/ml. This would suggest that 25-D blood levels up to 400 ng/ml might be safe.” — McCullough (2016)
After hearing this argument many, many times over the last year or so, it seems even sillier. Taking 360 times the vitamin D council’s recommended amount of cholecalciferol is not recommended, but the fact that it’s possible to accidentally do that — for months — shows how truly non-toxic cholecalciferol is.
Argument #4: “You Need The Active Form of Vitamin D to Activate The Vitamin D Receptor (VDR)”
Getting into cellular receptors is beyond my pay grade, but I will this one time.
Firstly, both 25-D and 1,25-D activate the vitamin D receptor, so this argument is a bit of a moot point.
But most importantly, as Gilbert Ling has pointed out, a hormone or signaling substance does not have to activate a specific receptor to exert its function:
“A receptor site as described in textbooks is distinguished by its steric adaptation to the specific drug molecule it reacts to. A familiar analogy often cited is the lock and key. Thus only structurally-fitting drugs can produce the desired pharmacological effect. Familiar as this model is, something vital to its function is missing.
In day-to-day experience, a fitting key does not do its job by just sitting there fitting. The fitting key must do something. That something, which the ordinary key usually does, is the mechanical act of ‘turning.’ There is no equivalent of this ‘turning’ in the conventional cell physiology or pharmacology. It is this basic deficiency, which might underlie Prof. Alfred Burger's complaint about medicinal chemistry cited in the opening page of this document.
In contrast, the association-induction hypothesis has offered from its very beginning, what is the equivalent o f that ‘turning,’ i.e., electronic polarization or induction.
[…]
…Clark's theory of drug action cannot readily answer the question of how the formation of a drug-effector complex can affect so many effector sites, some close, others far away. By demonstrating that the binding of one or more cardinal adsorbent(s) leads to across-the-board uniform change of near and far sites as if they were a single site, the Association-Induction Hypothesis offers a possible answer to this major unanswered question.”
— Life at The Cell and Subcellular Level by Gilbert Ling (2001)
So, rather than being a discrete mechanism through a hormone-receptor or drug-receptor complex, Ling’s view is that the electronic state (reduction-oxidation balance) of the cell governs the effects of drugs and hormones.
More specifically, Ling’s association-induction theory describes the living cell as a cooperatively linked protein-ion-water system that is maintained by the presence of cardinal adsorbents (carbon dioxide, ATP, steroids, ions, etc.) that are either electron-withdrawing or electron-donating. These cardinal adsorbents induce electronic conformations in proteins, which adsorb and structure cell water.
For example, take cancer, the prime feature of which is glycolysis, a reduced redox balance, lack of ATP, and altered water ordering that can be seen on an MRI:
“Longer T1 and T2 of the water protons in cancer cells are also in harmony with Albert Szent-Gyorgyi's prophetic announcement in 1957 in a footnote that cancer has ‘less water structure.’ His concept of ‘less water structure’ in cancer cells is compatible with the polarized multilayer theory…” — Ray Damadian (Inventor of MRI)
What does any of this have to do with 1,25-D activating the vitamin D receptor?
Firstly, it shows that overfocusing on a specific receptor is going to lead a person down a weird path — neglecting how a drug or hormone can change the activity of a cell’s affinity for water, or shift the balance of intracellular and extracellular ions, or act on mitochondria to impair energy production, or produce free radicals, or cause inflammation, etc.
Secondly, given my understanding of the hair follicle’s growth cycle and the vitamin D receptor’s (or cardinal site’s) involvement in the activation and proliferation of stem cells, I would infer that the vitamin D receptor is a type of regulatory material that supports cellular division— similar, to nitric oxide, histamine, and estrogen.
The Vitamin D Receptor in Growth and Differentiation
“When skin is injured, the stem cells are first activated to proliferate, and subsequently the progeny migrate and differentiate to regenerate the epidermis… the vitamin D receptor (VDR) is essential for these processes to occur… These results suggest that VDR is required for self-renewal, migration, and differentiation of epidermal stem cells and progeny during cutaneous wound healing.” — Oda, et al. (2018)
The key idea here is that that whole cell is a sensing organelle, creating specific receptors (or cardinal sites) as a “leverage point” (Ray Peat’s idea) to shift the cell in a particular direction based on its needs and available resources.
Argument #5: “You Need The Active Form of Vitamin D to Activate The Immune System”
This is another argument that seems compelling before you find out that you probably don’t want to activate your immune system.
In opposition to the traditional model of immunity, Polly Matzinger and Jamie Cunliffe describe the immune system as being more concerned with entities that do damage than with those that are foreign.
For example, when healthy tissues with a high rate of oxidative metabolism encounter a pathogen, they can simply do nothing and be tolerant of “otherness.” However, when cells and tissues are in a poor state of health, receiving proportionately less energy from oxidative metabolism, they are more likely to sound the alarm and mount an inflammatory immune response:
The Danger Model of Immunity
“I now believe that the ultimate power lies with the tissues. When healthy, tissues induce tolerance. When distressed, they stimulate immunity, and (continuing down this path) they may also determine the effector class of a response. Although it has long been thought that the effector class is tailored to the targeted pathogen (e.g., virus or worm), I now think that it is tailored to the tissue in which the response occurs.” — Polly Matzinger (2001)
The Mophostatic Model of Immunity
“...I have suggested that the core function of the immune (or morphostatic) system is to dispose of tissue debris (mess/non-mess discrimination) and restore order. The debris of degenerating cells provides a rich source of nutrients for micro-organisms. Could it be that the major goal of the immune system is to rapidly dispose of such debris?” — Jamie Cunliffe (2007)
If 1,25-D is the ‘immune response molecule,’ that’s just one more reason to limit its conversion by keeping the 25-D high, obtaining a generous amount of dietary calcium and magnesium, keeping the thyroid function up, etc.
Argument #6: “Taking a Vitamin D Supplement Gave Me Symptoms”
As I mentioned in the introduction, I empathize with anyone who took an oral supplement of vitamin D and felt like it harmed them.
In my estimation, people generally do not take seriously the idea that a “natural” supplement can cause serious harmful effects. Because of this, if a person were interested in trying cholecalciferol, I would recommend applying a form made from lanolin dissolved in olive oil to the skin.
If you’re still having issues with topical cholecalciferol, getting a generous amount of calcium (~2000 milligrams per day) and regularly eating eggs, ruminant liver, and canned oysters in olive oil might help since nutrients in those foods are needed for the hydroxylation of cholecalciferol by the liver.
Argument #7: “You’re Only Supposed to Get Vitamin D From The Sun”
As far as I know, it has never been claimed that a supplement of cholecalciferol can replace or is better than sunlight. For what it’s worth, for over a year, I’ve been climbing a rickety old ladder on the side of the casita I live in to layout whenever possible. If I fall off this ladder, I will likely break my neck — but to me, regular sunlight is worth the risk.
If a person were saying that all supplements, in general, are too risky and that a person should focus on food, sunlight, and whatever else they can do naturally to maximize function — I would disagree, but strongly empathize as I believe most supplements create more problems than they solve. However, if a person is going to promote this line of thinking, it should be consistent across the board.
From what I’ve seen, though, most anti-vitamin D proponents don’t feel this way regarding other supplements (e.g., magnesium, etc.). To single cholecalciferol supplements out, like they contain some extra level of danger, compared to supplements of magnesium, vitamin K, vitamin E, etc., is a mistake in my estimation.
Argument #8: “25-D Deficiency is Actually A Magnesium Deficiency”
This is a derivative of the ‘you need active vitamin D because the storage form is not biologically active’ argument:
“Vitamin D needs to be converted from its storage or inactive form 25-D to an active form 1-25-D before exerting its biological functions. These various stages of vitamin D conversions are actively dependent on the bioavailability of magnesium.” — Uwitonze, et al. (2018)
Speaking of magnesium — it’s important — and I think a person should try to construct their nutrition to include a regular source. Coffee, zucchini, and meat are all good sources of magnesium. Two to three cups of strong coffee per day can yield close to ~100 milligrams of magnesium per day, which is significant.



Moreover, if a person is worried about getting enough magnesium, they might want to take measures to assess their thyroid function, as Jerry Aikawa showed that cells cannot retain magnesium without enough thyroid:
"Thyroid hormone has a direct stimulatory action on the cellular transport of magnesium. A probable but not invariable result of hormonal stimulation of magnesium transport appears to be a preservation of normal cellular concentrations of magnesium..."— Magnesium: Its Biologic Significance by Jerry K. Aikawa (1981)
Argument #9: “Vitamin D Supplementation Depletes Vitamin A, Vitamin K, and Copper”
An important aspect of the bioenergetic point of view is that increasing the rate of metabolism can increase your nutritional requirements:
“In general, hyperthyroidism has been shown to increase the need for many dietary essentials, whereas hypothyroidism appears to ameliorate some dietary deficiencies." … "If marked changes in endocrine balance can induce or aggravate dietary deficiencies, optimal dietary supplementation should help to alleviate the resulting clinical picture.” — Harris, B., Ingle, D. Vitamins and Hormones Vol. 18. 1961.
If a person obtains a generous amount of metabolic stimulants such as calcium, vitamin D, sugars, red light, etc., they may immediately need more of the nutrition that eggs, ruminant liver, and canned oysters in olive oil contain.
However, since stress wastes and destroys various nutrients, getting the metabolic rate up can also help avoid malnutrition.
Regarding supplemental cholecalciferol causing deficiencies at physiological amounts — I couldn’t find anything, so if you, the reader, are aware of any articles about this topic, I would be interested in reading them in the comments.
Argument #10: “Vitamin D Has Gone Mainstream and is Part of an Agenda to Poison You”
I think there is an agenda to poison and kill people, but I haven’t seen anything that vitamin D was a part of that. If everything that reached the mainstream were harmful, aspirin and coconut oil would have to be added to that list. Vitamin K has been gaining a lot of traction recently, so maybe that’s toxic, too.
Argument #11: “Just Because a Substance Lowers a Stress Hormone Doesn’t Make it Good”
This is another point of contention that I agree with the spirit of. For example, supplemental estrogen can reduce the symptoms of menopause by destroying the pituitary and its release of gonadotrophins.
Matt Blackburn brought this point up on his Instagram not too long ago, suggesting that fluoride also decreased parathyroid hormone referencing a paper by Chen, et al. I couldn’t make much of the paper Matt linked, but I found a handful of other papers on the apparently well-known link between fluorosis and hyperparathyroidism that are referenced below.
Outro, Or: I’m Still The #1 Cholecalciferol Fan
If I were going to predict the anti-vitamin D people’s response to this article, I would guess that the context will immediately be ignored, followed by the addition of overwhelming complexity and obfuscation.
For what it’s worth, my life does not revolve around cholecalciferol supplementation being “good” or “bad” — it’s simply something that helped me gain a level of health that I didn’t have before.
When I see people in the health world with fanatical grievances, it doesn’t automatically discredit what they’re saying, obviously not, but it does make me skeptical of what exactly is going on.
Metabolic health is a multidisciplinary field, and extreme overspecialization often leads to extreme errors.
“The worst man of science is he who is never an artist, and the worst artist is he who is never a man of science. In early times, medicine was an art, which took its place at the side of poetry and painting; today they try to make a science of it, placing it beside mathematics, astronomy, and physics.” — Armand Trousseau (1869)
“For successful practice, a doctor has to be an artist armed with basic scientific knowledge in medicine.” — Panda, S.C. (2006)
If you enjoyed this post make sure to subscribe as I will be releasing exclusive uncensored content here in addition to The Generative Energy Podcast.
More References
Fluoride Increases PTH
“High fluoride ingestion has a definite relationship with increased parathyroid hormone secretion, which may be responsible for maintaining serum calcium levels and may have a role in toxic manifestations of fluorosis.” Gupta, et al. (2001)
“Fluoride, by interfering calcium balance, maybe the cause of secondary hyperparathyroidism.” — Koroglu, et al. (2010)
“The effect of fluoride on osteoclasts is less well understood than its effect on osteoblasts, and is complicated by a possible effect of fluoride-induced secondary hyperparathyroidism.” — Chachra, et al. (1999)
“Other diseases simulating radiographic features of fluorosis are… parathyroid hormone disorders…” — Fisher, et al. (1989)
“Secondary hyperparathyroidism has been suggested as a possible mechanism by which fluoride produces changes in bone, and hyperparathyroidism has been found in some humans and experimental animals exposed to fluoride.” — Kragstrup, et al. (1989)
“Metabolic bone disease occurred more frequently in residents of endemic (fluorosis) areas than in residents of nonendemic areas whose nutritional status was comparable. Common metabolic bone disorders, associated with endemic skeletal fluorosis, were osteoporosis (bone resorption), rickets, osteomalacia, and parathyroid bone disease.” — Teotia, et al. (1984)
“It appears that fluoride ingestion during lactation created a heightened state of calcium homeostatic stress. As a result, bone mineral was mobilized by resorption of the endosteal surface and by cavitation of the interior of the cortex. Secondary hyperparathyroidism is thought to play an integral part (in skeletal fluorosis) in an attempt to maintain calcium homeostasis.” — Ream, et al. (1983)
“The inhibition of resorptive function together with the decreased level at which bone and serum calcium equilibrate after the incorporation of fluoride would lead to a fall in serum calcium and a compensatory increase in parathyroid hormone secretion. This rise in serum parathyroid hormone would stimulate the differentiation of progenitor cells into both osteoblasts and osteoclasts.” — Ream, et al. (1983)
“Unopposed fluoride may lead to hyperparathyroidism” — Vigorita, et al. (1983)
“The increased bone resorption stimulated by fluoride administration may be due to excessive parathyroid activity.” — Riggins, et al. (1974)
“Fluoride administration in both man and animals has been shown to stimulate new bone formation. However, the bone is poorly mineralized, and osteomalacia and secondary hyperparathyroidism frequently occur.” — Jowsey, et al. (1972)
“The demonstrable hyperactivity of the parathyroid glands in fluorotic rabbits and sheep in the presence of this inhibition of resorption suggests that it is a compensatory phenomenon to maintain the serum calcium at a constant level.” — — Faccini, et al. (1969)











To me it sounds like you've built a ton of assumptions upon assumptions here. And I'd say the problem with this debate is that no one seems to be able to know when to just stop.
We entered hyperreality a long time ago. False can only become more false. So it doesn't matter how much we're all gonna be going on about this, it wont change what the truth is.
When you're going to call it a vitamin, when it's really a secosteroid, already there it changes the subconscious perception of what we're dealing with.
People who are 'anti vitamin D' aren't saying don't eat animal foods and to not go out in the sun. 'We' (I think it's not helpful to be dividing people into two groups, what happened to come to your own conclusions?) are arguing for the case that supplementing is unnecessary and can in fact be dangerous.
Haven't seen anyone mention sulfur metabolism, water solubility of all the many different metabolites of this secosteroid there seem to exist vs the form you supplement with.
How do you know the body has the capacity to be handling that and not see any negative consequences whatsoever? How much are we able to store in and release from our adipose tissues? How do we know that what is assumed to be a deficiency is a proven to have a causative relationship with people's hypothyroid symptoms and not just a downstream effect?
I could keep asking questions. I haven't found any answers, nor have anyone been able to answer them for me from what I've seen.
I don't think specificity is such a high government principle in the cell as we think it is. I think Pollack is right in that it comes down to the charge environment. Beyond that - aren't we just mostly guessing still? Another example we know is the mixed serotonin agonists and antagonists, that still don't seem to be understood very well? So does 'vitamin' D completely operate in isolation from everything else in the cell that affect the environment? Seems sulfate is very important here for one.
https://medium.com/@JosephGiacona/the-current-vitamin-d-craze-is-not-harmless-39f8fb3f8960
- I also ended up with the same debilitating back pain, couldn't work nor move for about a week and pain lingered for months, which I ascribe to lack of an inflammatory response to guide my immune system. Because I experienced something similar again after being careless with my eating, only this time the pain was completely gone after two days of letting things run their course (no aspirin either). An excessive inflammatory response is prob what you want to be guarded against. But I do think the body is being given way too little credit in being able to fix stuff on its own - just like it isn't trusted that it can figure out which D metabolites it might need when and where.
We have to start with establishing how we know:
1. what is real
2. what is the truth.
Otherwise you can just go on and on forever here, approximating reality so much that you'll eat your own tail. While looking out into reality and talking to people about their experiences gives a different picture (yes, I am one of those who stopped using it in various ways and got better from it).
I don't think anyone is going to have problems as such from using a few hundred IUs, but once we move into the thousands, that's where things get more murky. And let's not forget our default state is to NOT be taking this secosteroid as a 'supplement' to begin with.
I decided to stop supplementing 1.5 years ago until I could have a final answer as to what the truth here really is. I figured 2-3 years down the line would give me all the answers I ever needed (given that I live in Scandinavia and am dark skinned).
If you're interested, maybe you could dive into Selye's Calciphylaxis https://archive.org/details/in.ernet.dli.2015.141725/page/n3/mode/2up - I got a copy about a year ago, but personally just haven't had the time and as time passed, I lost interest in it because I started seeing improvements in symptoms after stopping.
'Poe imagines the situation in which a sailor, who has gone out on a fishing expedition, finds himself caught in a huge maelstrom or whirlpool. He sees that his boat will be sucked down into this thing. He begins to study the action of the ström, and observes that some things disappear and some things reappear. By studying those things that reappear and attaching himself to one of them, he saves himself. Pattern recognition in the midst of a huge, overwhelming, destructive force is the way out of the maelstrom. The huge vortices of energy created by our media present us with similar possibilities of evasion of consequences of destruction. By studying the patterns of the effects of this huge vortex of energy in which we are involved, it may be possible to program a strategy of evasion and survival. (...)'
- Marshall McLuhan
At the end of the day all we have to go by is pattern recognition. If it isn't consistent is isn't true. This debate is a great example of dichotomania. And we need to realize we are dealing in the abstract as well.
D3 supplementation changed my life: I went from one respiratory infection after another with the doctors saying they would only worsen with age. No physician ever suggested a test to determine my Vitamin D levels. Years later, respiratory infections are a thing of the past.